









































 Stroke and myocardial infarction with contemporary hormonal contraception
Stroke and myocardial infarction with contemporary hormonal contraception
Objective To evaluate the association between contemporary hormonal contraceptive use and the risk of incident ischaemic stroke and myocardial infarction.
Design Real-world, nationwide, prospective cohort study.
Setting Denmark, by use of national registries.
Participants All women aged 15-49 years residing in Denmark between 1996 and 2021, with no history of arterial or venous thrombosis, antipsychotics use, cancer, thrombophilia, liver disease, kidney disease, polycystic ovary syndrome, endometriosis, infertility treatment, hormone therapy use, oophorectomy, and hysterectomy.
Main outcome measures First time diagnosis of ischaemic stroke or myocardial infarction at discharge.
Results Among 2 025 691 women followed up for 22 209 697 person years, 4730 ischaemic strokes and 2072 myocardial infarctions occurred. Standardised ischaemic stroke rate per 100 000 person years were 18 (95% confidence interval 18 to 19) for no use, 39 (36 to 42) for combined oral contraception, 33 (25 to 44) for progestin-only pills, and 23 (17 to 29) for intrauterine device. Standardised myocardial infarction rate per 100 000 person years were 8 (8 to 9) for no use, 18 (16 to 20) for combined oral contraception, 13 (8 to 19) for progestin-only pills, and 11 (7 to 16) for intrauterine device. Compared with no use, current use of combined oral contraception was associated with an adjusted rate ratio of 2.0 (1.9 to 2.2) for ischaemic stroke and 2.0 (1.7 to 2.2) for myocardial infarction. These corresponded to standardised rate differences of 21 (18 to 24) extra ischaemic strokes and 10 (7 to 12) extra myocardial infarctions per 100 000 person years. Compared with no use, current use of progestin-only pills was associated with an adjusted rate ratio of 1.6 (95% CI 1.3 to 2.0) for ischaemic stroke and 1.5 (1.1 to 2.1) for myocardial infarction, equating to 15 (6 to 24) extra ischaemic strokes and four (−1 to 9) extra myocardial infarctions per 100 000 person years. Increased arterial thrombotic risk was also observed with use of the combined vaginal ring (adjusted incidence rate ratio of 2.4 (1.5 to 3.7) for ischaemic stroke and 3.8 (2.0 to 7.3) for myocardial infarction), patch (3.4 (1.3 to 9.1) and no myocardial infarctions), and progestin-only implant (2.1 (1.2 to 3.8) and ≤3 myocardial infarctions), whereas no increased risk was observed with progestin-only intrauterine device (1.1 (1.0 to 1.3) for ischaemic stroke and 1.1 (0.9 to 1.3) for myocardial infarction).
Conclusions Use of contemporary oestrogen-progestin and progestin-only contraceptives was associated with an increased risk of ischaemic stroke and, in some cases, myocardial infarction except for the levonorgestrel-releasing intrauterine device, which was not associated with either. Although absolute risks were low, clinicians should include the potential risk of arterial thrombosis in their assessment of the benefits and risks when prescribing a hormonal contraceptive method.
At least 248 million women worldwide are estimated to use hormonal contraception according to the World Health Organization.1 All currently marketed hormonal contraceptives have an acceptable and similar effectiveness in preventing unwanted pregnancies and safety is a key consideration when making clinical recommendations on which type of hormonal contraceptive to use.
Previous studies have suggested a potential increased risk of ischaemic stroke and myocardial infarction with use of hormonal contraception,234 but the evidence is inconsistent, with studies finding both no association and even a protective effect of hormonal contraception use.56
Most existing research has investigated the influence of only combined oestrogen-progestin oral contraceptives on arterial thrombosis risk without consideration of other types of contemporary hormonal contraceptives such as the combined vaginal ring, transdermal patch, progestin-only pills, intrauterine devices, subcutaneous implant, and intramuscular injection.356789101112 A single Danish cohort study published in 2012 examined the associated ischaemic stroke and myocardial infarction risk with different types of hormonal contraceptives and found a significantly increased risk with use of combined oral contraceptives and the vaginal ring.2 Although main estimates for some progestin-only contraceptives were indicative of an increased risk of ischaemic stroke and myocardial infarction, the study was insufficiently powered to conclude the direction of association for systemic progestin-only products.2
In this nationwide, prospective cohort study, we assessed the association of using contemporary hormonal contraceptives on the risk of incident ischaemic stroke and myocardial infarction according to oestrogen type, oestrogen dose, progestin type, mode of administration, and duration of use. The types of contraception that we considered were combined oestrogen-progestin pills, vaginal ring, and transdermal patch as well as progestin-only pills, intrauterine devices, subcutaneous implant, and intramuscular injection.
We conducted a nationwide prospective cohort study of all Danish women aged 15-49 years during 1996-2021 with no medical history of any arterial or venous thrombosis, cancer (except non-melanoma skin cancer), thrombophilia, liver disease, kidney disease, use of antipsychotics, infertility treatment, hormone therapy use, oophorectomy, hysterectomy, polycystic ovary syndrome, and endometriosis.
We followed up women from 1 January 1996, or from their 15th birthday if this occurred after the study began, and until 1 July 2021, emigration, death, or the occurrence of any arterial or venous thrombosis, cancer (except non-melanoma skin cancer), thrombophilia, liver disease, kidney disease, use of antipsychotics, infertility treatment, hormone therapy use, oophorectomy, hysterectomy, polycystic ovary syndrome, or endometriosis, whichever came first. Immigrated women entered the cohort five years after the date of immigration to ensure information on the eligibility criteria. Supplementary table S1 outlines the exact definitions of the exclusion and censoring criteria.
A unique personal identification number given to all Danish citizens at birth or on immigration was used to facilitate reliable data linkage across registries. We used six registries: (1) the Civil Registration System,13 which contains information about all Danish citizens’ sex, date of birth, and vital status since 1968; (2) the National Registry of Medicinal Product Statistics,14 which includes information on all redeemed prescriptions at Danish pharmacies since 1995; (3) the National Registry of Patients,15 which comprises information on discharge diagnoses and surgical procedures for all somatic admissions to hospital since 1976; (4) the Danish National Birth Registry,16 which holds information on all live and death births since 1973; (5) The Registry of Legally Induced Abortions,17 which includes information on all induced abortions in Denmark since 1973; and (6) Statistics Denmark,18 which provides a yearly update on the education status for all Danish citizens.
Women were classified as current users of hormonal contraception if they filled a prescription for any hormonal contraceptive. The National Registry of Medicinal Product Statistics provided daily updated, individual level data for all redeemed prescriptions of hormonal contraception throughout the study period, including the date of redemption, type, and quantity of the contraceptive.14
Women were considered exposed to hormonal contraception from the date of prescription redemption. For hormonal contraceptives taken orally, via a vaginal ring, patch, or injection, the duration of use was calculated based on the number of daily doses purchased. For long acting reversible contraceptives, such as subcutaneous implants and intrauterine devices, we assumed a duration of use one year shorter than the maximum approved period to account for potential early discontinuation. All prescriptions were extended by 28 days to accommodate possible delays in initiation. Gaps longer than 28 days between prescriptions were considered a time of no use. Exposure time was paused if a woman filled a prescription for a different hormonal contraceptive or became pregnant. In a sensitivity analysis, we excluded the first four weeks after the acquisition of a new hormonal contraceptive to address challenges in determining which product might be responsible for any arterial thrombotic events during product transitions.
A comprehensive list of contemporary hormonal contraceptives available during the study period, along with their anatomical therapeutic chemical codes, is provided in supplementary table S2.
Incident cases of ischaemic stroke and myocardial infarction were identified using the Danish National Patient Registry and the National Danish Registry of Causes of Death. Ischaemic strokes were classified according to the International Classification of Diseases, 10th revision (ICD-10) codes I63 and I64, while myocardial infarction was identified using ICD-10 code I21.1519
Time updated information about age, calendar time, educational level, pregnancy, surgery, use of oral tranexamic acid, and comorbidities was available for the entire study population (supplementary table S1).
Information about comorbidities, including hypertension, diabetes, hypercholesterolaemia, atrial fibrillation, and atrial flutter, was retrieved for all included women from The Danish National Patient Registry and The National Registry of Medicinal Product Statistics (supplementary table S1).
To reduce potential bias from the temporary confounding effect of pregnancy, surgery, and the use of tranexamic acid, women were temporarily censored and did not contribute with person time and events to the analysis during these periods.
The Danish Medical Birth Registry provided information on all births undergone by the cohort, and a woman was censored temporarily during pregnancy, for six months after delivery, and for 12 weeks after other types of pregnancy terminations, which were identified through The Danish National Patient Registry and The Registry of Legally Induced Abortions (supplementary table S1).
From the Danish National Patient Registry, we retrieved information about all surgeries. If a woman was admitted to hospital for at least one day due to surgery, she would be temporarily censored from the date of surgery until eight weeks following her discharge date (supplementary table S1).
To further strengthen our analysis of the impact of hormonal contraceptive use on arterial thrombotic risk, we also implemented a temporary censorship of women using the antifibrinolytic tranexamic acid, which is potentially thrombogenic, and prescribed for heavy menstrual bleeding. Women were temporarily censored for eight weeks from the date of tranexamic acid prescription redemption (supplementary table S1).
If a woman had an event, died, emigrated, or met any permanent censoring criterion during a period of temporary censoring, she was permanently censored from the date of the given incident.
Data for family history was available only for women whose parents had resided in Denmark from midlife onward. A woman was classified as having a family history of thrombosis if her mother had a thromboembolic event before age 60 or her father before age 55.
Information about smoking status and body mass index was only available for parous women from the Danish Medical Birth Registry, which collects data for body mass index and smoking status just before pregnancy for women who have given birth from the year 2004 and onwards.
We used Poisson regression to estimate the adjusted incidence rate ratio of ischaemic stroke and myocardial infarction with current use of the different types of hormonal contraceptives. All models were adjusted for age in one year intervals and calendar year in five year intervals as well as educational level, hypertension, diabetes, hypercholesterolaemia, and atrial fibrillation or flutter. No use constituted the reference group in all primary analyses.
We conducted a sensitivity analysis to further mitigate the potential for user bias, whereby users of hormonal contraception may have an elevated baseline risk of arterial thrombotic events, independent of the contraceptive itself. We used person time for former hormonal contraception users (defined as those who had discontinued use for at least six months) as the reference group.
To eliminate potential carryover effects from prior hormonal contraceptive use, we conducted an additional sensitivity analysis. In this analysis, women were censored at the time that they discontinued their first hormonal contraceptive, ensuring that only person time related to their initial product was included. The study period for this analysis began in 2000, providing a minimum of five years of exposure history before study entry. Only women with no history of hormonal contraceptive use during this period were included. Women who had not redeemed a prescription for hormonal contraception contributed to the never-use exposure category, which was the reference group.
We calculated incidence rates of ischaemic stroke and myocardial infarction standardised by age, calendar time, and education, per 100 000 person years using the distribution of these factors in the entire cohort as the standard. Standardised incidence rate differences were calculated for each type of hormonal contraceptive with no use as the reference.
In a subcohort of women with data for family history of thrombosis, further adjustment for family history was made. In a subpopulation of parous women with the information available, further adjustments of smoking and body mass index were made. Analyses were repeated in the age strata of younger than 35 years and 35 years or older. The effect of duration of hormonal contraception use was also investigated. The durations were categorised based on uninterrupted periods of use, with categories defined as less than a year, one to four years, and more than four years. Women contributed person time and events to the relevant duration category based on the length of their uninterrupted use. Data were managed with SAS software, version 9.4,20 and analysed using R software version 4.2.1.21
Other than the women of reproductive age included in the research group, no patients or members of the public were involved in the design, analysis, or reporting of this study, as the project lacked funding for patient and public involvement initiatives.
A total of 2 025 691 women aged 15 to 49 years contributed with 22 209 697 person years of follow-up time (fig 1). During follow-up, 4730 incident ischaemic strokes and 2072 incident myocardial infarctions occurred. A total of 93 (2.0%) women who developed ischaemic stroke and 185 (8.9%) women who had a myocardial infarction died within 30 days from diagnosis.



हुज़ैफ़ा अबरार March 03 2025 0 7770
आयशा खातून March 06 2025 0 3330
एस. के. राणा March 06 2025 0 2664
एस. के. राणा March 07 2025 0 1998
एस. के. राणा March 08 2025 0 1554
हुज़ैफ़ा अबरार March 03 2025 0 7770
आयशा खातून March 06 2025 0 3330
एस. के. राणा March 06 2025 0 2664
एस. के. राणा March 07 2025 0 1998
एस. के. राणा March 08 2025 0 1554
हुज़ैफ़ा अबरार March 03 2025 0 7770
British Medical Journal February 25 2025 0 4440
आयशा खातून March 06 2025 0 3330
एस. के. राणा March 06 2025 0 2664
एस. के. राणा March 07 2025 0 1998
एस. के. राणा March 08 2025 0 1554
 सौंदर्य
सौंदर्य
सौंदर्या राय May 06 2023 0 75690
सौंदर्या राय March 09 2023 0 80972
सौंदर्या राय March 03 2023 0 78993
admin January 04 2023 0 79266
सौंदर्या राय December 27 2022 0 69981
सौंदर्या राय December 08 2022 0 59440
आयशा खातून December 05 2022 0 111444
लेख विभाग November 15 2022 0 82696
श्वेता सिंह November 10 2022 0 91632
श्वेता सिंह November 07 2022 0 81131
लेख विभाग October 23 2022 0 66023
लेख विभाग October 24 2022 0 67463
लेख विभाग October 22 2022 0 74406
श्वेता सिंह October 15 2022 0 81126
श्वेता सिंह October 16 2022 0 76355

किशोरों को लगने वाले टीकों और साठ साल या उससे अधिक आयु के लोगों को दिए जाने वाली एहतियाती खुराक संबं
कोरोना वायरस के संक्रमण से 2,887 और लोगों के जान गंवाने से मृतकों की संख्या 3,37,989 पर पहुंच गई जबक
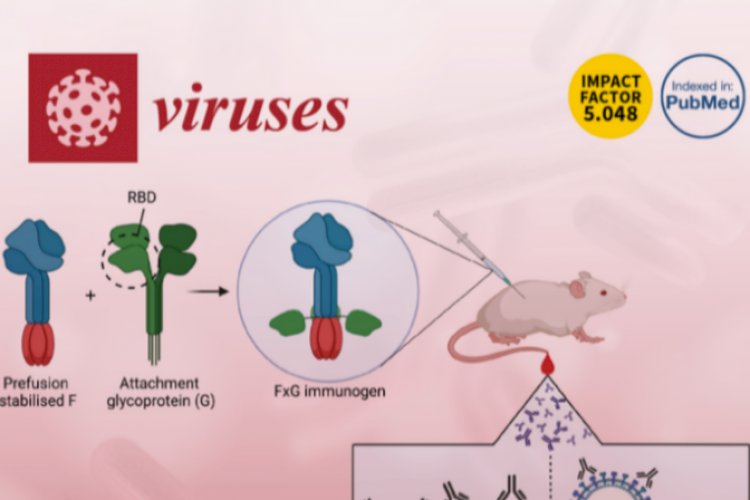
पुणे स्थित नेशनल इंस्टीट्यूट ऑफ वायरोलॉजी (एनआईवी) की वरिष्ठ वैज्ञानिक डॉ. प्रज्ञा यादव के अनुसार को

तीसरे चरण के क्लिनिकल ट्रायल ज़ेनिक्स, जिसका आयोजन जॉर्जिया, मोलदोवा, रूस और दक्षिण अफ्रीका की 11 साई

राज्यपाल आनंदीबेन पटेल ने राजभवन स्थित प्रज्ञाकक्ष में नैक ग्रेडिंग के लिए पहली बार तैयारी कर रहे सं

एम्स में मरीजों को एमआरआई स्कैन के लिए लंबा इंतजार नहीं करना होगा। दिल्ली एम्स में मरीजों को अब एमआर

विश्व हेपेटाइटिस दिवस के अवसर पर होप इनिशिएटिव तथा इंडियन मेडिकल एसोसिएशन लखनऊ और निर्वान हॉस्पिटल द

सहारा हॉस्पिटल के मानसिक रोग विशेषज्ञ डॉक्टर अपूर्वा उपाध्याय ने इस गम्भीर मानसिक समस्या के बारे में

देश में मेडिकल शिक्षा और स्वास्थ्य का सबसे बड़ा संस्थान, एम्स भी अब बिलासपुर की शान बढ़ा रहा है। बिल

फाइलेरिया की दवा खाने के बाद महिला की हालत खाराब हो गई। परिजन आनन फानन में महिला को लेकर जिला अस्पता

COMMENTS